 |
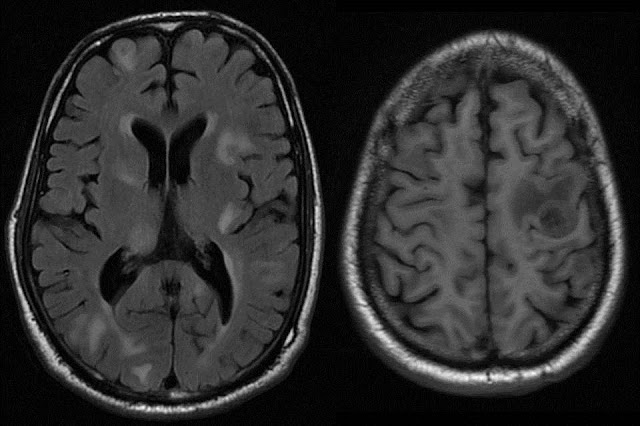
| Axial T2 FLAIR images showing diffuse hypointensity of bilateral frontoparietal white matter with sparing of subcortical U fibres. There is sparing of perivascular white matter giving a "TIGROID" or "LEOPARD SKIN" appearance |
 |
Axial and Sagittal T2 Wt images show extent of hyperintense signal in bilateral fronto temporo parieto occipital white matter from deep periventricular region to subcortical region
with sparing of U fibres. |
 |
Axial DWI and sagittal T1 Wt images: Mild restricted diffusion noted along the advancing edge of dysmyelination. Note the involvement of distal body and splenium of corpus callosum
in the disease process on T1 Wt image. |
Classification of Leukodystrophies:
·
Metachromatic leukodystrophy is an autosomal recessive disorder
caused by a deficiency of the lysosomal enzyme arylsulfatase A.
·
This enzyme is necessary for formation of myelin sheath.
·
In metachromatic leukodystrophy, sulfatides accumulate in various
tissues, including the brain, peripheral nerves, kidneys, liver, and
gallbladder.
·
The accumulation of sulfatides within glial cells and neurons
causes the characteristic metachromatic reaction.
·
Metachromatic leukodystrophy is diagnosed biochemically on the
basis of an abnormally low level of arylsulfatase A in peripheral blood
leukocytes and in urine.
·
Three different types of metachromatic leukodystrophy are
recognized according to patient age at onset:
1.
Late infantile
2.
Juvenile
3.
Adult
·
The most common type is late infantile metachromatic
leukodystrophy, which usually manifests in children between 12 and 18 months of
age and is characterized by motor signs of peripheral neuropathy followed by
deterioration in intellect, speech, and coordination.
·
Within 2 years of onset, gait disturbance, quadriplegia,
blindness, and decerebrate posturing may be seen.
·
Disease progression is inexorable, and death occurs 6 months to 4
years after onset of symptoms.
·
At T2-weighted MR imaging, metachromatic leukodystrophy manifests
as symmetric confluent areas of high signal intensity in the periventricular
white matter with sparing of the subcortical U fibers.
·
No enhancement is evident at computed tomography or MR imaging.
·
The tigroid and “leopard skin” patterns of demyelination, which
suggest sparing of the perivascular white matter, can be seen in the
periventricular white matter and centrum semiovale.
·
The corpus callosum, internal capsule, and corticospinal tracts
are also frequently involved.
·
The cerebellar white matter may appear hyperintense at T2-weighted
MR imaging.
·
In the later stage of metachromatic leukodystrophy,
corticosubcortical atrophy often occurs, particularly when the subcortical
white matter is involved.
Reference : Leukodystrophy
in Children: A Pictorial Review of MR Imaging Features, May 2002 RadioGraphics,
22, 461-476.







_page23_image1.png)







